We make HCC coding education easy.
DoctusTech’s expert HCC coding services offer the best way for clinicians to learn HCC coding.
9 out of 10 doctors prefer DoctusTech to any other method of HCC training – find out why.
If you are interested in a trial of our HCC Coding Mobile App, please share your information below and we will respond right away.
DoctusTech’s expert HCC coding services offer the best way for clinicians to learn HCC coding.
9 out of 10 doctors prefer DoctusTech to any other method of HCC training – find out why.


in RAF accuracy.

with clinicians.


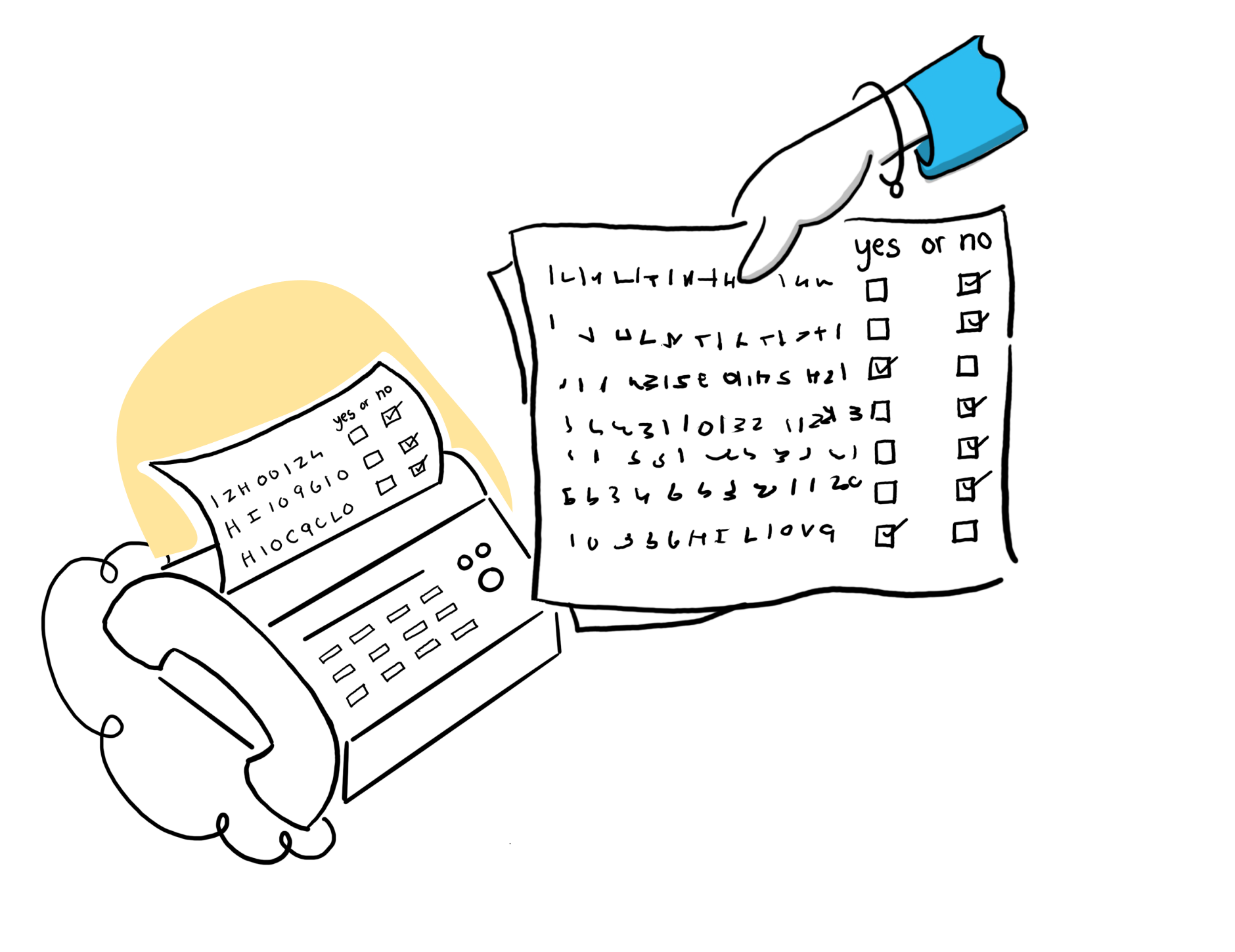
Lectures, emails, memos, and coder-led feedback.
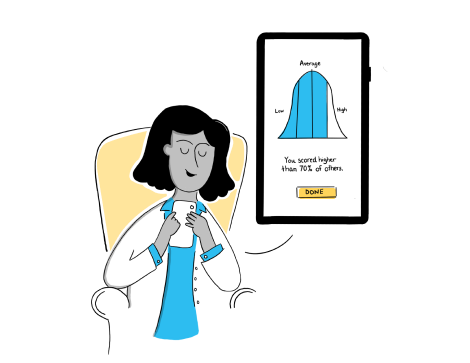
Five minutes of app-based, asynchronous learning.
 >
> 
Making it easier for clinicians to provide accurate documentation.
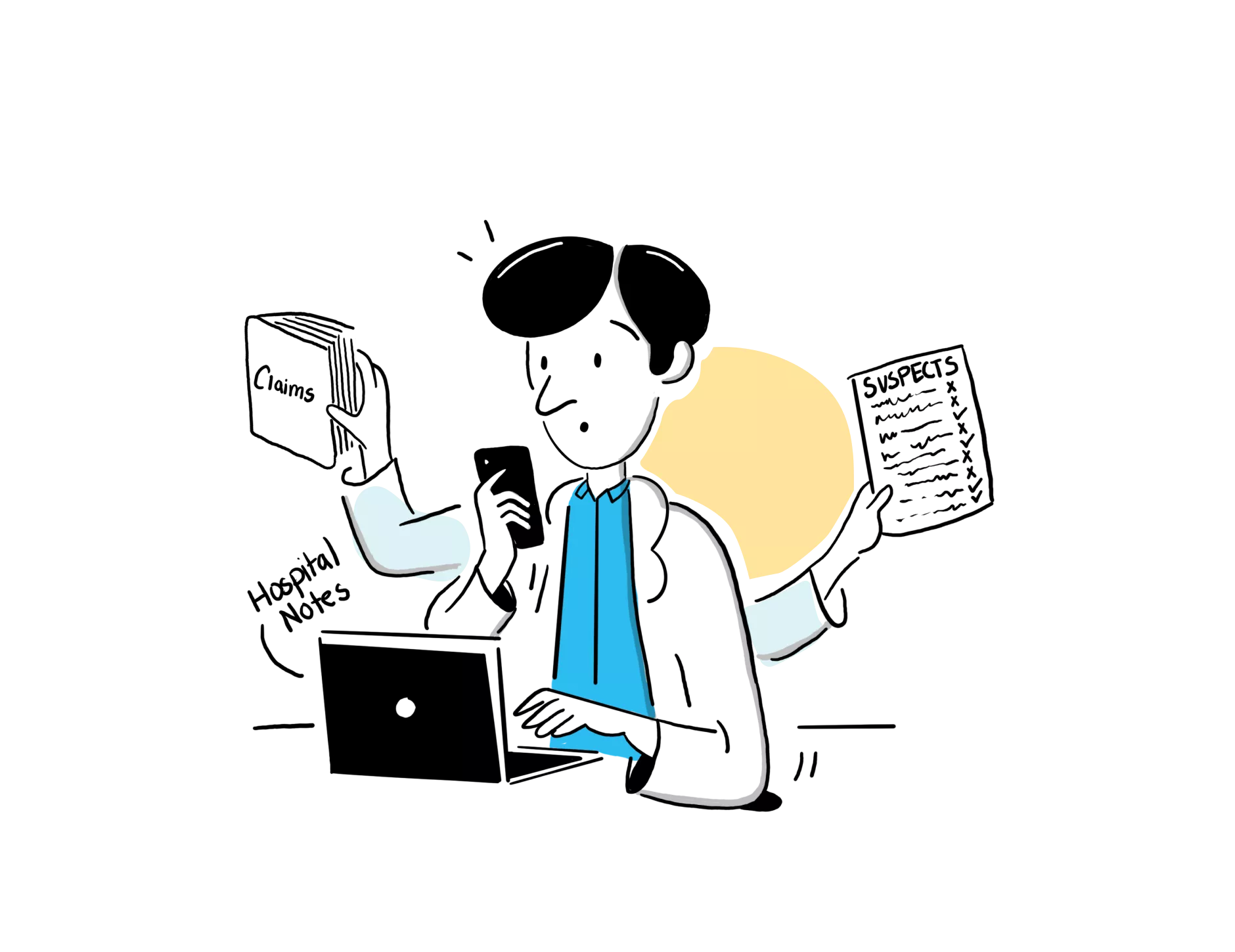
Manually review payor suspect lists, specialist claims data, lab reports, and other forms of unstructured information.
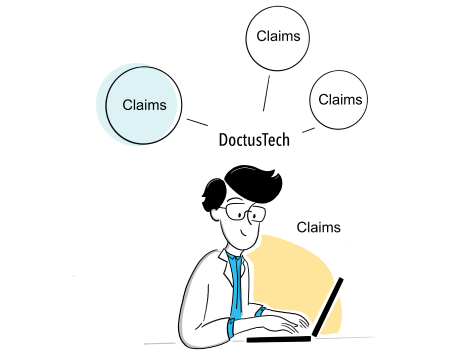
Aggregate all external data sources to create a single source of truth in your EMR of choice.
 >
> 
Access better data – not more data – at the point of care.
Cast a broad net, waste time sifting through unsupported diagnoses.
High-specificity, review-supported diagnoses.







“
I like the way they ask the questions, because it's like I'm sitting for boards...There are a lot of other programs out there, but not like this.
“
The mobile app is wonderful, in that it's a clinical vignette — it's what is literally in front of their face, and it gets them thinking.
“
This is more intuitive and is full of 'ah-ha moments,' whereas all of my other education on this topic hasn't really been that iterative or intuitive. So I do like the format.
