We asked VBC thought leaders to share their experiences of fee-for-service and value-based reimbursement models.
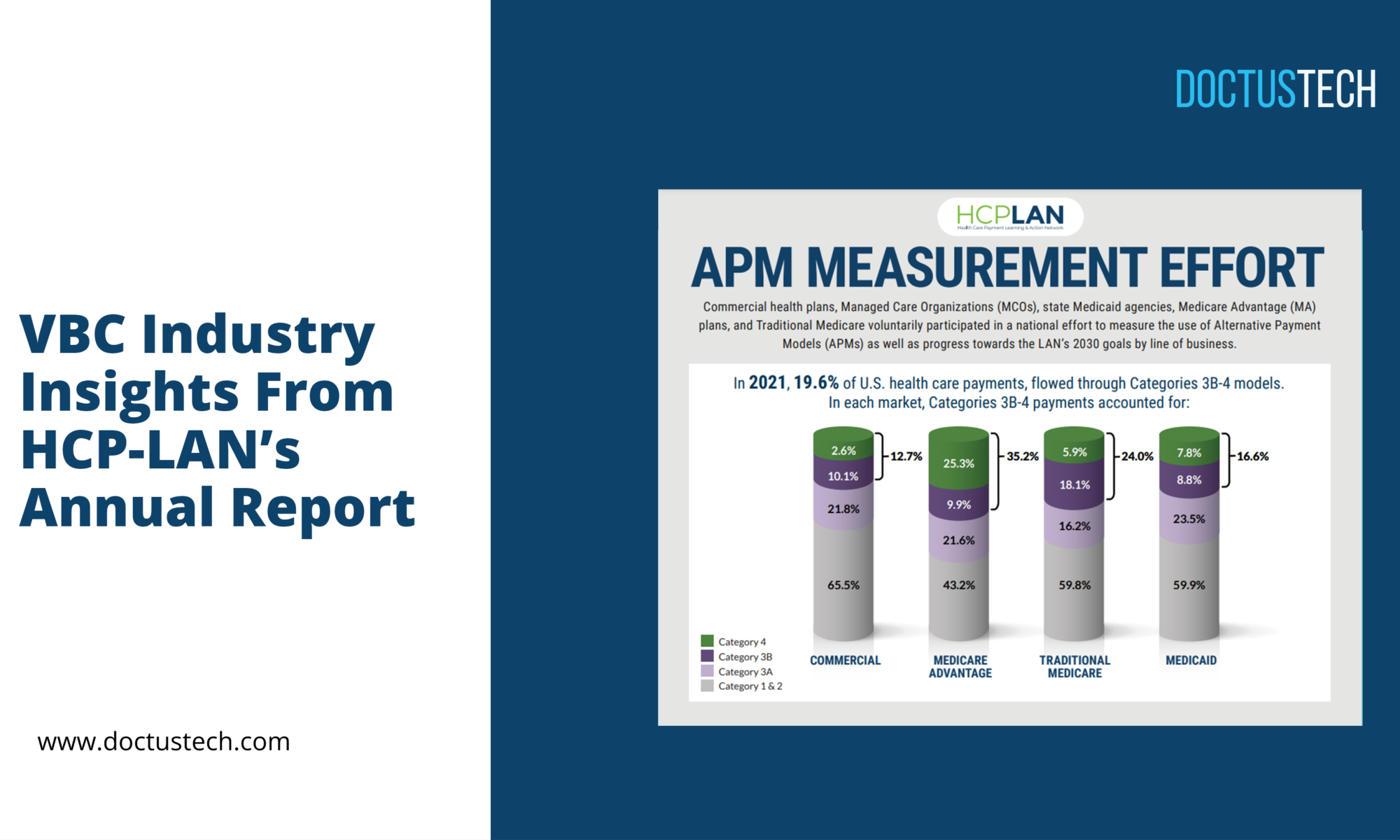
While value-based payment models are on the rise in the U.S, primary care practices still receive the majority of their payments via fee-for service. In 2022, 70% of primary care physicians reported receiving fee-for-service payments, versus just 46% for value-based payments. Although many health systems are now transitioning to the value-based care model, this transition can’t happen overnight – meaning some combination of both value-based and fee-for-service models is inevitable. In this article, we’re going to explore so-called blended payments in value-based care, and ask whether organizations should persist with them long-term.
Are value-based care and fee-for-service incompatible?
Value-based care and fee-for-service are often considered to be polar opposite reimbursement models. While the fee-for-service model sees providers receive payment for each service they deliver – regardless of the quality of care or patient outcomes – value-based medicine follows the equation of ‘value = quality ÷ cost’. That means, under the VBC reimbursement model, providers are rewarded for delivering high-quality care and positive patient outcomes – while effectively managing costs.
In the highly-politicized U.S healthcare landscape, it’s possible to see value-based care and fee-for-service medicine as philosophically incompatible. “The difference is the basic premise of having a transactional relationship with a healthcare provider, versus putting the responsibility of the outcome of that relationship on the healthcare provider,” says Dr. Rayny Ramirez, CEO, Community Medical Group. “At the clinical level, doctors can care less about financials and cost. Doctors just want to be doctors.”
Blended payment: a marriage of inconvenience
The transition to value-based healthcare slowed during the turmoil imposed by the COVID-19 pandemic, but this was never a rapid process to begin with. Medical Economics describes how the industry has “inched toward” value-based healthcare over the last decade “on an incremental basis”. This slow shift has left many organizations in a kind of limbo, forced to operate blended payment models comprising both value-based and fee-for-service payments. Although a marriage of convenience, these blended payment models could potentially explain recent criticism of VBC success rates, says the Chief Clinical Officer of a leading at-risk physician group who prefers to remain anonymous.
“I wonder if they’re trying to do both,” she tells us. “I wonder if they’re trying to do this treadmill of fee-for-service and – ‘oh yeah, I have to slow down to see my VBC patient’. It’s impossible.”
“I always equate it [blended payment] to a cross-training sneaker: it’s not good for running, it’s not good for playing tennis. If you want to run, you wear a running shoe, and if you want to play tennis, you wear a tennis shoe.”
Both of our experts have experienced the blended payment method first hand, and both have questions about its efficacy as a long-term solution.
“I’ve been in an organization that’s fee-for-service, I’ve been in an organization that is value-based, and I’ve been in an organization that is both at the same time – or trying to be both at the same time – which is kind of crazy,” says Dr. Ramirez.
“It is really hard to do both well,” the CCO agrees. “And I think that’s why some providers don’t necessarily see the value in value-based care – because they just see the documentation requirements and preventative care checklists, and say ‘this is harder medicine’. They’re not looking at the outcomes.”
Reaping the benefits
Both of our interviewees extol the virtues of working for dedicated value-based care organizations over the blended model. “I love our health center because we’re just a running shoe!” the CCO laughs. “I think certain providers say their VBC programs haven’t been successful because they’re living with one foot in each world.”
Dr. Ramirez agrees. “It’s all relative to how you measure the value of VBC,” he tells us. “In my previous stewardship – with a different organization that provided care for senior patients – we were able to improve or extend life by an average five years in seniors with a certain number of conditions. Potentially the costs are higher, but what’s the price of living five more years?”
Both parties are realistic regarding the challenge of transitioning to value-based care. “I’m not going to pretend that there aren’t more rigorous documentation requirements in value-based care,” the CCO says. “The documentation is intimidating. And it wasn’t something that providers learned in medical school… If you’re used to commercial documentation, you might be like, ‘this is a burden’.”
Accurate documentation starts with education. Clinicians, MAs, coders and other staff must buy into the increased burden of documentation necessitated by the switch to value-based care, before learning the many intricacies of risk adjustment and HCC coding. The DoctusTech HCC coding education app applies active learning theory to engage clinicians at 90%, and encourage lasting behavior change with 75% knowledge retention. It’s the preferred method of HCC education for 9/10 clinicians – ensuring users not only retain the valuable information they’re taught, but that they’re motivated to keep learning for the long term.
If you need help managing the transition to value-based care, get in touch and arrange a demo of the DoctusTech app today.